The cardiac system, a vital component of human physiology, is a complex muscular organ that pumps blood through the body, ensuring oxygen and nutrient delivery to tissues.
Overview of the Cardiovascular System
The cardiovascular system, also known as the circulatory system, is a closed network responsible for transporting blood throughout the body. It consists of the heart, arteries, veins, and capillaries, working together to deliver oxygenated blood to tissues and deoxygenated blood to the lungs. The heart acts as the central pump, while blood vessels serve as the pathways for blood circulation. This system is divided into two main circulations: systemic, which supplies oxygenated blood to the body, and pulmonary, which carries deoxygenated blood to the lungs for oxygenation. Efficient functioning of the cardiovascular system is essential for maintaining life and overall health.
Importance of the Cardiac System in Human Physiology
The cardiac system plays a central role in human physiology by maintaining the continuous circulation of blood, ensuring the delivery of oxygen and nutrients to cells and the removal of waste products. It regulates body temperature, supports immune function, and enables the transport of hormones and signaling molecules. A functioning cardiac system is crucial for energy production, physical activity, and overall organ function. Its failure can lead to severe health complications, emphasizing its importance in sustaining life and maintaining homeostasis within the body.

Anatomy of the Heart
The heart is a muscular, cone-shaped organ located near the midline of the thoracic cavity, weighing between 7 and 15 ounces, essential for blood circulation.
Chambers of the Heart
The heart contains four chambers: the right and left atria, and the right and left ventricles. The atria are the upper chambers that receive blood returning to the heart, while the ventricles are the lower chambers that pump blood out to the lungs and the rest of the body. A thin, fibrous septum separates the right and left sides of the heart, preventing mixing of oxygenated and deoxygenated blood. Valves within the chambers ensure blood flows in one direction, maintaining efficient circulation. This structural organization is crucial for the heart’s function in maintaining systemic and pulmonary circulation.
Layers of the Heart Wall
The heart wall is composed of three distinct layers: the epicardium, myocardium, and endocardium. The epicardium is the outermost layer, serving as a protective membrane that surrounds the heart and attaches it to the diaphragm. Beneath it lies the myocardium, the thick muscular layer responsible for the heart’s contractions and pumping action. The innermost layer, the endocardium, lines the heart’s chambers and valves, ensuring smooth blood flow and preventing clot formation. Together, these layers work in harmony to maintain the heart’s structural integrity and functional efficiency, enabling it to pump blood effectively throughout the body.
Heart Valves and Their Functions
The heart contains four valves that ensure blood flows in one direction through its chambers. The atrioventricular valves (tricuspid and mitral) are located between the atria and ventricles, preventing backflow during ventricular contractions. The semilunar valves (pulmonary and aortic) are situated at the exits of the ventricles, ensuring blood moves forward into the pulmonary artery and aorta, respectively. These valves are crucial for maintaining efficient blood circulation, preventing backflow, and ensuring oxygenated and deoxygenated blood are directed appropriately. Their proper functioning is essential for maintaining cardiac efficiency and overall circulatory health, enabling the heart to pump blood effectively to meet the body’s needs.
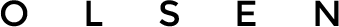
The Conduction System of the Heart
The heart’s conduction system is a specialized network of cells that initiates and coordinates the heartbeat. It begins with the sinoatrial (SA) node, the heart’s natural pacemaker, located in the right atrium. The SA node generates electrical impulses, which travel to the atrioventricular (AV) node, delaying the signal to ensure proper atrial contraction. The impulse then moves through the Bundle of His to the ventricles, spreading through Purkinje fibers to trigger synchronized contractions. This system ensures a consistent and rhythmic heartbeat, maintaining proper timing and coordination between atrial and ventricular contractions. It is essential for efficient blood circulation and overall cardiac function.
The Pericardium and Its Role
The pericardium is a fibroserous sac surrounding the heart, providing protection and support. It consists of two layers: the outer fibrous pericardium and the inner serous pericardium, which secretes fluid to reduce friction during heartbeats. The pericardium restricts excessive heart movement, anchoring it within the thoracic cavity. It also contains the heart within the mediastinum, preventing displacement and maintaining its position. Additionally, the pericardium aids in cushioning the heart against external shocks and infections. Inflammation of the pericardium, known as pericarditis, can impair its function, potentially leading to cardiac complications; Overall, the pericardium plays a crucial role in maintaining cardiac stability and function.
Blood Circulation
Blood circulation is vital for delivering oxygen and nutrients to tissues while removing waste products. It involves the systemic and pulmonary systems, ensuring efficient blood flow throughout the body.
Pulmonary Circulation
Pulmonary circulation refers to the movement of blood between the heart and lungs, enabling gas exchange. Deoxygenated blood from the right ventricle flows through the pulmonary artery to the lungs, where it picks up oxygen and releases carbon dioxide in the alveoli. Oxygen-rich blood returns to the left atrium via the pulmonary veins. This system operates at lower pressure than systemic circulation, ensuring efficient gas exchange. The pulmonary arteries and veins form a network surrounding the bronchi, facilitating this critical process. Pulmonary circulation is essential for maintaining proper oxygenation of blood and overall bodily function, making it a vital component of the cardiac system.
Systemic Circulation
Systemic circulation is the network of arteries, veins, and capillaries that transports oxygenated blood from the left ventricle to tissues and deoxygenated blood back to the heart. The left ventricle pumps blood into the aorta, the largest artery, which branches into smaller arteries supplying organs and tissues. Oxygen and nutrients diffuse into cells through capillaries, while deoxygenated blood collects in veins, returning to the right atrium. This high-pressure system ensures efficient delivery of oxygen and removal of waste products, regulated by the autonomic nervous system and local factors to meet the body’s metabolic demands, maintaining homeostasis and overall health.
The Cardiac Cycle
The cardiac cycle refers to the sequence of events during a heartbeat, involving systole (contraction) and diastole (relaxation), ensuring blood is pumped and the heart is refilled.
Phases of the Cardiac Cycle
The cardiac cycle consists of two main phases: systole and diastole. Systole includes isovolumetric contraction, ventricular ejection, and isovolumetric relaxation. Diastole comprises rapid filling, diastasis, and atrial contraction. These phases ensure efficient blood pumping and ventricular refilling, maintaining cardiac efficiency and proper blood circulation throughout the body.
Factors Affecting Heart Rate
Heart rate is influenced by various factors, including the autonomic nervous system, hormones, physical activity, and emotional state. The sympathetic nervous system increases heart rate, while the parasympathetic system decreases it. Hormones like adrenaline and thyroid hormones also enhance heart rate. Physical activity stimulates an increase to meet oxygen demand, while stress and anxiety can elevate it. Age, gender, and overall health additionally play roles, with younger individuals typically having higher resting heart rates. Pathological conditions, such as heart disease or electrolyte imbalances, can also alter heart rate, making it a critical indicator of cardiovascular health and overall physiological state.

Blood Pressure Regulation
Blood pressure regulation involves baroreceptors, blood volume, and vascular tone, ensuring optimal circulation and organ perfusion through dynamic physiological adjustments.
Mechanisms of Blood Pressure Control
Blood pressure regulation involves a complex interplay of neural, hormonal, and local mechanisms. Baroreceptors in blood vessels detect changes in pressure and activate the autonomic nervous system. The renin-angiotensin-aldosterone system responds to low blood volume or pressure by increasing vasoconstriction and fluid retention. Sympathetic stimulation increases heart rate and vascular resistance, while parasympathetic activity promotes relaxation. Local factors, such as endothelial-derived nitric oxide, cause vasodilation, reducing resistance. These mechanisms ensure precise control of blood flow and maintain homeostasis, adapting to physiological demands and preventing hypertension or hypotension.
Role of the Renin-Angiotensin-Aldosterone System
The renin-angiotensin-aldosterone system (RAAS) is a critical regulator of blood pressure and fluid balance; Renin, released by the kidneys, triggers the conversion of angiotensinogen to angiotensin I. Angiotensin I is converted to angiotensin II by angiotensin-converting enzyme (ACE), primarily in the lungs. Angiotensin II is a potent vasoconstrictor and stimulates the adrenal cortex to release aldosterone. Aldosterone promotes sodium retention in the kidneys, increasing blood volume and pressure. RAAS activation compensates for low blood pressure or volume, maintaining cardiovascular homeostasis. Dysregulation of this system is linked to hypertension and heart disease, making it a target for therapeutic interventions like ACE inhibitors and ARBs.
The Autonomic Nervous System and the Heart
The autonomic nervous system regulates cardiac function through sympathetic and parasympathetic branches, modulating heart rate and contraction strength to maintain homeostasis during rest and activity.
Sympathetic and Parasympathetic Nervous System Influence
The sympathetic nervous system increases heart rate and contraction strength, preparing the body for stress, while the parasympathetic nervous system promotes relaxation, slowing heart rate via the vagus nerve. Both systems regulate cardiac function through opposing actions, maintaining homeostasis. Sympathetic stimulation activates adrenergic receptors, enhancing cardiac output, whereas parasympathetic activity releases acetylcholine, reducing heart rate and promoting rest. This dual control ensures the heart adapts to varying physiological demands, such as exercise or rest, maintaining optimal performance and overall cardiovascular health.

Coronary Circulation
The coronary arteries arise from the aorta, supplying oxygenated blood to the myocardium, while coronary veins return deoxygenated blood to the right atrium, ensuring cardiac tissue nourishment.
Arterial Supply to the Heart
The heart receives its arterial supply primarily through the left and right coronary arteries, which originate from the ascending aorta. The left coronary artery branches into the anterior descending artery and the circumflex artery, supplying the left ventricle, septum, and lateral walls. The right coronary artery supplies the right atrium, right ventricle, and, in most individuals, the posterior descending artery. These arteries deliver oxygenated blood and nutrients to the myocardium, ensuring proper cardiac function. Obstruction of these arteries can lead to ischemia or infarction, highlighting their critical role in maintaining heart health and overall cardiovascular function.
Venous Drainage of the Heart
The venous drainage of the heart is primarily facilitated by the coronary sinus and its tributaries. The coronary sinus, located on the posterior surface of the heart, collects deoxygenated blood from the myocardium through the great, middle, and small cardiac veins. This blood is then emptied into the right atrium, completing the coronary circulation cycle. Proper venous drainage is essential for maintaining cardiac function, as it ensures the removal of metabolic waste and the recycling of blood through the heart. Any obstruction in this system can lead to cardiac dysfunction, emphasizing its importance in overall cardiovascular health and efficiency.
The Enteric Nervous System and Cardiac Function
The enteric nervous system (ENS), often referred to as the “little brain” of the gut, plays a significant role in modulating cardiac function. While primarily managing digestive processes, the ENS communicates with the central nervous system (CNS) through the vagus nerve. This bidirectional interaction influences heart rate variability and blood pressure regulation. For instance, during gastrointestinal stress, the ENS can signal the CNS to activate sympathetic responses, increasing cardiac activity. Conversely, parasympathetic signals from the ENS via the vagus nerve can promote relaxation and reduce heart rate; This intricate connection highlights the gut-heart axis as a critical area of study in cardiovascular health.
Cardiac Macrophages and Their Role
Cardiac macrophages are essential immune cells residing in the heart, playing a dual role in maintaining cardiac physiology and responding to pathology. They regulate tissue repair, inflammation, and immune responses, ensuring myocardial homeostasis. In physiological conditions, macrophages promote angiogenesis and support cardiac remodeling. During cardiac injury, such as myocardial infarction, they orchestrate the inflammatory response, clearing debris and facilitating healing. However, dysregulation of macrophages can contribute to pathological processes like fibrosis and heart failure. Their plasticity allows them to adapt to environmental cues, making them a focal point for understanding heart disease mechanisms and developing therapeutic strategies to modulate cardiac inflammation and repair.
Reactive Oxygen Species in Cardiac Redox Signaling
Reactive oxygen species (ROS) are chemically reactive molecules containing oxygen, playing a critical role in cardiac redox signaling. Derived from mitochondrial activity, NADPH oxidases, and other cellular sources, ROS regulate cellular processes like growth, differentiation, and apoptosis. In the heart, ROS modulate ion channel function, contraction, and vascular tone. However, excessive ROS levels can lead to oxidative stress, damaging cellular components and contributing to cardiovascular diseases. The renin-angiotensin-aldosterone system amplifies ROS production, exacerbating cardiac injury. Antioxidant systems, such as glutathione and superoxide dismutase, counterbalance ROS to maintain redox homeostasis, highlighting the importance of ROS signaling in both physiological and pathological cardiac conditions.
The cardiac system is a fascinating and essential organ, playing a central role in maintaining life by pumping blood throughout the body. Its intricate structure, including chambers, valves, and the conduction system, ensures efficient blood circulation. Understanding its anatomy, physiology, and regulation is crucial for appreciating its function in health and disease. Imbalances in mechanisms like blood pressure regulation or redox signaling can lead to cardiovascular disorders. Maintaining a healthy lifestyle and addressing risk factors are vital for preserving cardiac function. The heart’s resilience and adaptability make it a remarkable organ, and ongoing research continues to uncover its complexities and improve therapeutic strategies.